lv venting Venoarterial extracorporeal membrane oxygenation (VA-ECMO) increases left ventricular (LV) afterload, potentially provoking LV distention and impairing recovery. LV mechanical unloading (MU) with intra-aortic balloon pump (IABP) .
1972 OMEGA SEAMASTER DEVILLE. SKU: OME921. $0.00. Out of Stock. PRODUCT INFO. Circa: 1972. Model: Seamaster De Ville. Caliber: 563. Movement serial #: 34478118. Jewel count: 17 jewels. Movement type: Automatic wind. Case model: 166.020. Case material: Solid stainless steel. Case gasket: Does not take a gasket. Crystal: Original .
0 · va ecmo vs impella
1 · lvad vs ecmo
2 · lv venting vs unloading
3 · lv venting strategy
4 · lv venting myocarditis
5 · lv vent cardiac surgery
6 · left ventricular vent catheter
7 · left ventricular unloading
Rolex Datejust — Five-digit references. In 1977, Rolex introduced the 16xxx generation of references, commonly referred to as the five-digit generation. The same popular bezel styles remained: The smooth-bezel ref. 1600 became ref. 16000; The fluted-bezel ref. 1601 became ref. 16014 in steel and ref. 16013 in two-tone
Venoarterial extracorporeal membrane oxygenation (VA ECMO) is an established method of short-term mechanical support for patients in cardiogenic shock, but can create left .
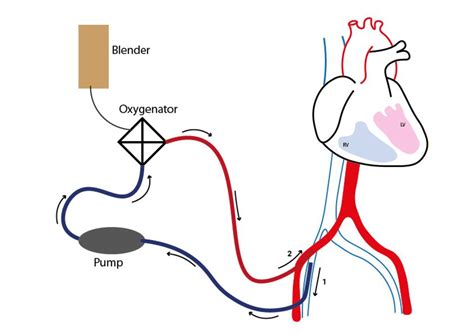
Several mechanical circulatory strategies can be used to achieve LV unloading or venting if conservative measures prove to be insufficient. Each method is associated with its own contraindications, risks, costs, and potential . LV venting refers to techniques or methods that reduce LV filling pressures. LV unloading refers to any intervention that reduces myocardial oxygen consumption, which is . LV venting, especially if done early (<12 hours), appears to be associated with an increased success of weaning and reduced short-term .Indications to vent the LV are variable and can be based on clinical, hemodynamic, or echocardiographic findings of impaired LV unloading, LV .
Venoarterial extracorporeal membrane oxygenation (VA-ECMO) increases left ventricular (LV) afterload, potentially provoking LV distention and impairing recovery. LV mechanical unloading (MU) with intra-aortic balloon pump (IABP) .LV venting, especially if done early (<12 hours), appears to be associated with an increased success of weaning and reduced short-term mortality. Future studies are required to delineate .
LV venting is an important adjunct of myocardial protection during systemic cooling before successful delivery of cardioplegia. Conventionally, LV vent is placed via the right superior .The LV vent is connected with an ‘underwater’ seal [F] via a ⅜ – ¼ connector to the ¼ inch LV tubing and then via the Y connector oxygenated blood enters the access limb of the ECMO circuit [G]. Imaging of the LV vent. .
LV unloading/venting was performed in 43.0% patients, of which intra-aortic balloon pump (IABP) was used in 48 (87.3%) patients, atrial transseptal venting in three (5.5%) patients, and both in four (7.3%) patients. Of note, no other LV unloading/venting strategies were adopted, as microaxial flow pump devices (mAFP) are not currently approved .
To Vent or Not to Vent: The Critical Role of Left Ventricular Venting With Extracorporeal Membrane Oxygenation Support Cardiovascular Revascularization Medicine, 10.1016/j.carrev.2022.04.011, 40: 142-143, Online .LV venting, especially if done early (<12 hours), appears to be associated with an increased success of weaning and reduced short-term mortality. Future studies are required to delineate the importance of any or early LV venting adjuncts on mortality and morbidity outcomes.During the following 12 to 72 hours, the decision to place an LV vent is based on the periodic (every 12 hours) assessment of the following conditions: 1) absent aortic valve opening; 2) arterial pulse pressure value <15 mm Hg; and 3) wedge pressure value >30 mm Hg. If 2 or more of these criteria are present, a trial of low-dose dobutamine .
Optimal patient selection and timing for LV venting remains uncertain because few robust prospective studies have evaluated this question. 27, 28 Commonly cited indications for LV venting include LV distension, an elevated PCWP, a low or absent pulse pressure, a lack of aortic valve opening, North–South syndrome, pulmonary edema, and lung . Alternatively, it has been proposed to anticipate temporary LV assist-device implantation upon initiation of VA ECMO, including adequate LV venting. 66,69 In this sense, it can be considered to use a large-sized LV apical vent with a minimum of a 32-F drainage cannula. Venous drainage of the VA ECMO circuit can be accomplished by percutaneous .Minimally invasive LV venting with CentriMag LVAD and ECMO. We have developed a minimally invasive approach to LV venting through the use of a CentriMag ventricular assist device (VAD) integrated with ECMO . In brief, this combines venous drainage from the femoral or jugular vein with drainage from the LV apex, and they are connected with . The LV vent was inserted during ECMO cannulation, and repeat echocardiography post venting showed a reduction in LV size compared to patients who did not undergo decompression . Patients with a vent also had significantly higher 30-day survival (55% versus 25%, P=0.034), though there was no difference in mortality at 12 months and there were no .
To date, there are several possibilities to decrease the likelihood of left ventricular distension on ECMO, but the cohort of patients who benefit from left ventricular venting is unclear. Decreasing afterload leads to a decrease in workload and O 2 consumption. In case of an extremely poor left ventricular function, it is advisable to .In previously published reports, variables of LV vent indication are the following. 1) An elevated pulmonary capillary wedge pressure, 2) a distended LV as seen on echocardiography, 3) an AV that remains closed during the cardiac cycle, 4) persistent pulmonary edema as seen on chest radiography, and 5) refractory ventricular arrhythmia. 11, 12Percutaneous cannulas that are placed from the femoral vein or the internal jugular (IJ) vein to the pulmonary artery (PA) can be used as inflow to an extracorporeal circuit as a left ventricular (LV) vent or as outflow for right ventricular assist device (RVAD) configuration. 1 They are easily and rapidly deployable with transesophageal and fluoroscopic guidance. 2, 3 In experienced .Inserting an ascending aortic vent would also be problem atic in the elderly with a fragile or calcified aorta. Venting through the pulmonary artery is an indirect, retrograde method which avoids the potential complications of direct LV apical venting and is considered to be adequate (3). LV venting through
This commentary refers to ‘Prevention and treatment of pulmonary congestion in patients undergoing venoarterial extracorporeal membrane oxygenation for cardiogenic shock’ by E. Lüsebrink et al., doi: 10.1093/eurheartj/ehaa547 and the discussion piece ‘Percutaneous left ventricular unloading in veno-arterial extracorporeal membrane oxygenation’, by M. Pozzi et .Left ventricular venting has many physiologic and prac- tical benefits. A venting technique is described that employs a simple, closed system which allows the per- fusionist to monitor left ventricular distention. By mon- itoring the left ventricular volume the perfusionist can regulate the degree of negative pressure on the vent and .
One such debate relates to the need for and the optimal timing and type of a left ventricular (LV) venting strategy to counteract the potential overloading effects on the left ventricle that can occur during VA ECMO support. . Grandin E.W., . The left ventricular (LV) vent is commonly inserted via the right superior pulmonary vein (RSPV) and directed toward the LV cavity through the mitral valve. We report a rare case in which the tip of the LV vent was misplaced into the aortic root across the aortic valve. An 88-year-old man was scheduled to undergo the Bentall procedure. After initiation of . All-cause mortality outcomes in relation to left ventricular (LV) venting during veno-arterial extracorporeal life support (VA-ECLS). 50–62,64–86 Overall, short-term (up to 30 days) mortality was reported in 755 or 1453 patients .Heterogeneous indications for LV unloading were reported. The selected literature was divided into subgroups, according to the location or the performed procedure for LV venting. Results: Case reports or case series accounted for 60% of the papers, while retrospective study represented 29% of them. Adult series were present in 67%, paediatric .

A surgically placed LV vent through the right upper pulmonary vein or left atrium and merged with vaECMO venous drainage provides significant decompression of the overloaded LV. Alternatively, a transseptal cannula in the left atrium can be implanted and connected to the venous ECMO cannula [ 12 ].
va ecmo vs impella
LV unloading/venting was performed in 43.0% patients, of which intra-aortic balloon pump (IABP) was used in 48 (87.3%) patients, atrial transseptal venting in three (5.5%) patients, and both in four (7.3%) patients. Of note, no other LV unloading/venting strategies were adopted, as microaxial flow pump devices (mAFP) are not currently approved . No statistically significant differences in terms of hemolysis, bleeding, renal failure, and stroke were observed. 29 This was further corroborated by the work of Truby et al, which showed that myocardial recovery was higher in patients without left ventricular distention, prompting the need for LV venting. 30 They also identified .
In the absence of surgical venting options or an Impella device, a pigtail catheter can provide a safe LV vent option. Case: A 54-year-old male presented to a non-surgical primary percutaneous coronary intervention (PCI) center with anterior ST-segment elevation myocardial infarction (STEMI) complicated by ventricular tachycardia (VT) arrest . Tepper and colleagues compared direct LV unloading with connection with the venous circuit of ECMO versus Impella (N = 45) and found similar mortality but a better reduction in pulmonary diastolic pressure in the direct LV vent group . In general, the ideal option will depend on patients’ comorbidities, available vascular accesses and . Other trials comparing routine left ventricular unloading with left-sided Impella implantation and no unloading are ongoing (REVERSE [A Prospective Randomised Trial of Early LV Venting Using Impella CP for Recovery in Patients With Cardiogenic Shock Managed With VA-ECMO], NCT03431467; UNLOAD ECMO [Left Ventricular Unloading to Improve Outcome .
Routine use of left ventricular vent is controversial in patients undergoing open heart surgery. However, surgeons use it during valvular surgery to maintain a dry field to make the operation easier. In addition it helps to prevent left ventricular .
LV venting is becoming increasingly important or applied. Thus, we strongly believe that adding a specification of the venting modality into the nomenclature of ECMO configuration should be advisable. The agreed method to add this specification might be a relevant task for ELSO and related organizations.

audemar piguet cheapest

A common sight back in the 1970s, the Adidas Bamba trainers are less common now, so a reissue is nice to see. Designed as an all-rounder and as a football shoe for hard ground, this Adidas Bamba trainers reissued in black and white variations - .
lv venting|left ventricular unloading